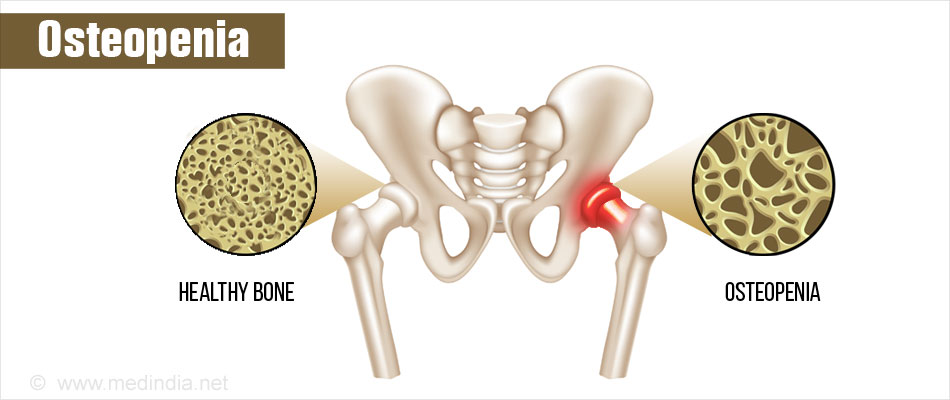
Osteopenia is a condition that begins in people who lose bone mass, and this results in weak bones. It is associated with low-calcium diets, smoking, age-related hormone changes, certain diseases, and medications. Women over 50 face higher risks of developing osteopenia and those diagnosed with the condition are at increased risk of developing osteoporosis, a serious medical condition that leads to bone fragility. It’s important to note that lifestyle changes may help slow bone loss and that beneficial treatments do exist. A special non-invasive X-ray test can measure the amount of calcium and other minerals in a segment of bone, typically the hips and spine, to diagnose bone health.
Symptoms of advanced osteopenia may include back pain, loss of height, a stooped posture, and easily fractured bones. However, these warning signs are usually only evident once the condition progresses. Osteopenia is detected via testing to include both a physical examination and a DEXA (dual-energy X-ray absorptiometry) imaging test. The DEXA test is painless and determines whether a person has healthy bones or osteopenia or osteoporosis. Patients are given a score called a T-score to indicate normal bone density, osteopenia, or osteoporosis. (The scoring is as follows: +1 to -1 = normal bone density, -1 to -2.5 = osteopenia -2.5 or lower = osteoporosis.) The test can also give healthcare providers a baseline measurement so that they can make future comparisons.
It’s important to be proactive when it comes to health. If you believe that you are at risk of osteopenia or osteoporosis, it’s vital to see a medical doctor to discuss testing and strategies to keep your bones healthy and strong. If a doctor concludes that you have osteopenia following testing, he or she may suggest some measures to keep bones healthy and prevent the onset of osteoporosis. This may include:
- Taking calcium and vitamin D supplements together. Note that calcium is a natural mineral that plays a role in the body’s bone formation process. Vitamin D helps the body absorb calcium.
- Eating a healthy and well-rounded diet full of nutritious fruits, vegetables, and calcium-rich foods.
- Performing daily exercise to include some type of weight training. Note that numerous studies show that weight-bearing exercise can help to slow bone loss, and some conclude that it can even build bone.
- Avoid unhealthy activities such as smoking. Also limit alcohol intake. Also, watch sugar intake as a diet high in sugar may drive both calcium and vitamin D deficiencies, per a study shared by Missouri Medicine.
Since people with low bone density are at increased risk of breaking bones, injury prevention is a critical step. Cleveland Clinic explains, “Falls are the leading cause of fractures in people with low bone density.” Thus, it’s vital to take personal safety measures to prevent falling. They suggest making sure homes have ample lighting, railings on stairs and in showers, and non-skid rugs. They also propose treating slippery surfaces indoors and out and removing tripping hazards from the home.
How Can a Physical Therapist Help?

A physical therapist can help you prevent and treat low bone mass at any age. They will prescribe the specific amount and type of exercise that best builds and maintains strong bones.
Your physical therapist will review your health history, including your medical, family, medication, exercise, dietary, and hormonal history. They will also conduct a complete physical examination and identify your risk factors for low bone density.
It is important to exercise throughout life. It is especially important to exercise to maintain healthy bones if you have been diagnosed with low bone mass. Exercise can help to build bone or slow the loss of bone mass.
Your physical therapist is likely to prescribe exercise and physical activity to help prevent fractures and falls, and to reduce bone loss. Your treatment program may include:
Exercise focus
- Posture guidance (spinal alignment and awareness for fracture prevention).
- Balance training.
- Leg strengthening.
- Spine stretches.
- Hip stretches.
Weight-bearing exercises
- Dancing.
- Tai chi.
- Walking at a quick pace (122-160 steps per minute, or 2.6 steps per second).
- Jumping, stomping, heel drops.
- Running.
- Racket sports.
Resistance exercises
- Weightlifting.
- Use of resistance bands.
- Gravity-resistance exercises (such as pushups, stair climbing).
_______________________________________________________
sources:
amac.us/osteopenia-what-women-over-50-should-know
choosept.com/guide/physical-therapy-guide-osteopenia-low-bone-mass
The National Osteoporosis Foundation recommends people at average risk get a DEXA scan starting at 65 for women and 70 for men. The onset of symptoms, frequent bone fractures, and/or a family history of bone fractures or osteoporosis may also increase one’s risk for bone loss. This may necessitate a DEXA scan at a younger age. As always, it’s important to dialogue with your doctor regularly regarding all aspects of your health, including the all-important bones that support your body, allow you to move, and protect your brain, heart, and organs from harm.
Please note that this article is for general information purposes only and is not intended as medical advice.